IRS Releases Final 2017 ACA Reporting Forms and Instructions
November 1, 2017
Overview
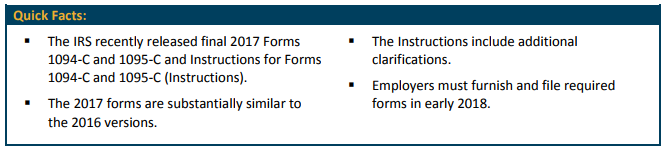
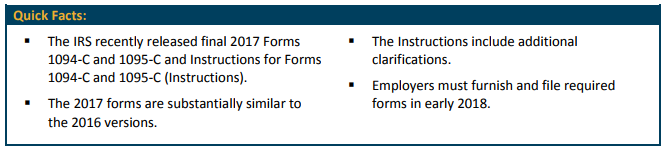
Recently, the Internal Revenue Service (IRS) released 2017 forms and instructions for reporting required under Internal Revenue Code (Code) Sections 6055 and 6056.
Reporting entities, including health insurance carriers and self-insured plan sponsors that are not applicable large employers (ALEs), use Forms 1094-B and 1095-B to report information required under Section 6055.
ALEs use Forms 1094-C and 1095-C to report information required under Section 6056, as well as information required under Section 6055 for ALEs who sponsor self-insured plans.
Background
The Affordable Care Act (ACA) created reporting requirements under Code Sections 6055 and 6056. Under these rules, certain employers must provide information to the IRS about the health plan coverage they offered (or did not offer) or provided to their employees in the prior calendar year. Each reporting entity must annually file all of the following with the IRS:
an individual statement (generally Form 1095-C, for employers) for each person who was provided with minimum essential coverage (for providers reporting under Section 6055), or for each full-time employee (for ALEs reporting under Section 6056); and
a transmittal form (generally Form 1094-C, for employers) for all of the returns filed for a given calendar year.
Key changes
The 2017 forms are substantially similar to the 2016 versions. The biggest difference is that the new forms and instructions delete all references and sections relating to expired transition relief that is unavailable to any employers in 2017.
Section 4980H Transition Relief. Some employers could have relied on certain transition relief to avoid potential penalties under specific circumstances under Code Section 4980H for the 2015 plan year (including any portion of the 2015 plan year that fell in 2016). However, no such relief applies in 2017. Thus, the IRS removed references to Section 4980H transition relief from the Instructions. In addition, the IRS revised Form 1094-C to remove references to this transition relief. Specifically, the following two sections on Form 1094-C related to this transition relief have been designated as “Reserved” and should not be used: Part II, in the “Certifications of Eligibility” Section on Line 22, Box C; and Part III, in the “ALE Member Information – Monthly” table, column (e).
Instructions for Recipient. Form 1095-C (and Form 1095-B – mostly used by carriers) includes an “Instructions for Recipient” section which states, “For additional information about the tax provisions of the Affordable Care Act (ACA), including the individual shared responsibility provisions, the premium tax credit, and the employer shared responsibility provisions, see www.irs.gov/Affordable-Care-Act/Individuals-and-Families or call the IRS Healthcare Hotline for ACA questions (1-800-919-0452).”
Updated Penalty Amounts. The Instructions include updated penalty amounts for failures to file returns and furnish statements. The adjusted penalty amount is $260 per violation, with an annual maximum of $3,218,500 (up from a maximum of $3,193,000, for 2016).
Code Series 2 (Section 4980H Safe Harbor Codes and Other Relief). The Instructions clarify that there is no specific code to enter on line 16 to indicate that a full-time employee who was offered coverage either did not enroll or waived the coverage.
Corrected Forms 1095-C. The Instructions include additional information for employers that have errors on Forms 1095-C. Specifically, the instructions indicate that Forms 1095-C filed with incorrect dollar amounts on line 15, Employee Required Contribution, may fall under a safe harbor for certain de minimis errors. The safe harbor generally applies if no single amount in error differs from the correct amount by more than $100. If the safe harbor applies, employers will not have to correct Form 1095-C to avoid penalties. However, if the recipient elects for the safe harbor not to apply, the employer may have to issue a corrected Form 1095-C to avoid penalties. For more information, see IRS Notice 2017-9.
Format of Returns Filed with the IRS. The Instructions clarify that all reporting entities must print all returns filed with the IRS in landscape format.
“Plan Start Month” box. A prior draft version of 2017 Form 1095-C clarified that the “Plan Start Month” box in Part II of Form 1095-C will remain optional for 2017. The Instructions indicate that this box may be mandatory for the 2018 Form 1095-C.
Due dates
Reporting entities must furnish individual statements (Form 1095-B or 1095-C, or a substitute form) to all full-time employees as well as any individuals covered under self-insured health plans on or before January 31 of the year immediately following the calendar year to which the statements relate. Reporting entities must file Form 1094 and Forms 1095 with the IRS by February 28 if filed by paper, and by March 31 if filed electronically. In 2018, electronic filings are due by April 2 since March 31 is a Saturday.
Extensions of time for filing
In general, reporting entities may receive an automatic 30-day extension of time to file returns with the IRS by submitting Form 8809, Application for Extension of Time To File Information Returns, by the due date of the returns. No signature or explanation is required for the extension. Under certain hardship conditions reporting entities may apply for an additional 30-day extension. See the instructions on Form 8809 for more information. According to the IRS, information returns may continue to be filed after the filing deadline (both on paper and electronically). Employers that missed the filing deadline should continue to make efforts to file their returns as soon as possible.
Electronic filing with the IRS
Any reporting entity that will file at least 250 Forms 1095-B or 1095-C with the IRS must do so electronically. The 250-or-more requirement applies separately to each type of return and separately to each type of corrected return. For IRS Forms 1094-C and 1095-C that are filed electronically, transmitters must use “AIR,” the Affordable Care Act Information Return system.
Additional resources
The IRS previously released the following materials which provide helpful guidance for employers subject to the reporting rules. Although the materials relate to the 2015 forms, most of the information remains relevant for 2017.
Q&As on Section 6055 and Q&As on Section 6056; and
A separate set of Q&As on Employer Reporting using Form 1094-C and Form 1095-C.
Recommended steps for employers
Ensure a thorough understanding of the ACA employer shared responsibility rules and terminology, and the purpose of the forms.
Review the instructions!
Be ready: prepare with your payroll and reporting providers, designate a project manager, capture data for each month in 2017, review current systems capabilities, and conduct testing.
Know what codes and options to use in the forms, such as affordability safe harbor codes and coverage indicators.
If you are filing electronically in-house, be sure to register and follow the steps outlined on the AIR website.
If you are part of an ALE group, carefully review the ALE group reporting rules.
EPIC Employee Benefits Compliance Services For further information on this or any other topics, please contact your EPIC benefits consulting team. EPIC offers this material for general information only. EPIC does not intend this material to be, nor may any person receiving this information construe or rely on this material as, tax or legal advice. The matters addressed in this document and any related discussions or correspondence should be reviewed and discussed with legal counsel prior to acting or relying on these materials